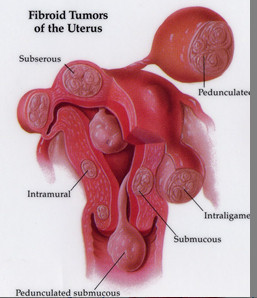
A myomectomy is a surgery to remove fibroids without taking out the healthy tissue of the uterus. It is best for women who wish to have children after treatment for their fibroids or who wish to keep their uterus for other reasons. You can become pregnant after myomectomy. But if your fibroids were imbedded deeply in the uterus, you might need a cesarean section to deliver. Myomectomy can be performed in many ways. It can be major surgery (involving cutting into the abdomen) or performed with laparoscopy or hysteroscopy. The type of surgery that can be done depends on the type, size, and location of the fibroids. After myomectomy new fibroids can grow and cause trouble later.
Video of Hysteroscopic Myomectomy
No incision Fibroid Removal
There are 3 main types of Myomectomy procedures:
Hysteroscopic myomectomy
In this procedure, a camera is introduced through the vagina and into the uterine cavity. Submucous or intracavitary myomas are easily visualized and can be resected or removed using a wire loop or similar device. While submucous myomas can cause significant bleeding and anemia, their management is straightforward with hysteroscopic myomectomy. Patients usually are sent home after surgery and have minimal need for recovery.
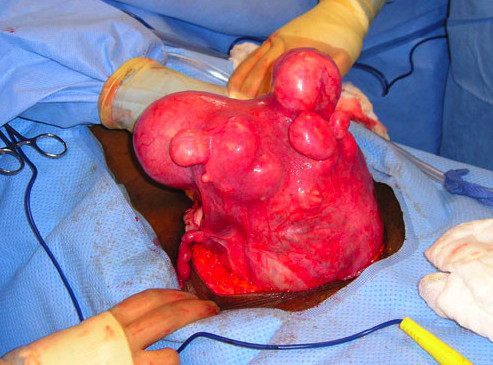
Open myomectomy
Now reserved for patients with very large myomas, an open myomectomy is traditional surgery involving an incision similar to a cesarean section incision. The fibroids are shelled out from the normal uterus and the uterus is repaired using multiple rows of suture. Patients normally are hospitalized for 1-3 days and experience discomfort similar to other open surgeries. Most patients are able to return to work in 4 weeks comfortably.
Laparoscopic or Robotic myomectomy
During this procedure, a 10 millimeter (1 centimeter) camera is introduced, usually through the umbilicus or belly button. Three other small (5 – 8mm) incisions are made and instruments are used to complete the surgery similar to an open myomectomy. This procedure is more time consuming, and technically difficult but affords the patient a more rapid recovery. In our practice, patients are observed in the hospital overnight and usually released in the morning. They typically return to work in 2-4 weeks. The da Vinci robotic system has revolutionized laparoscopic myomectomy, allowing for improved suturing of the uterus with better visualization. See the section on robotic surgery for more information.
Risks of Myomectomy
Although early studies suggested that the rate of morbidity associated with myomectomy was increased compared with hysterectomy, subsequent research suggests that the risks of the two procedures are similar (26-28). Clinical experience and pooled results of numerous small studies suggest that abdominal myomectomy significantly improves menorrhagia symptoms (overall 81% resolution; range 40-93%), with similar results for resolution of pelvic pressure (29). Therefore, abdominal myomectomy is a safe and effective option for treatment of women with symptomatic leiomyomas.
However, women choosing myomectomy face the risk of recurrence of leiomyomas. A number of studies have examined the use of ultrasonography to assess the recurrence risk of leiomyomas after abdominal myomectomy, but the accuracy of the estimate depends on the sensitivity of the measuring instrument (10, 30-32). Studies have indicated that women who experience childbirth after a myomectomy appear to have a decreased recurrence risk (30, 31). There have been conflicting reports over whether the preoperative use of GnRH agonists affects recurrence risk (10, 32).
The clinically relevant endpoint is whether a second surgical procedure is needed after conservative surgery. In a relatively large series (125 patients monitored at least 5 years and up to 23 years), there was evidence that recurrence depended on the number of leiomyomas present. Of those women who had a single leiomyoma, 27% had recurrent tumors and 11% required hysterectomy. Of those women who had multiple leiomyomas, 59% experienced recurrent tumors. Of the women in the multiple leiomyoma group, 26% required repeat myomectomy, hysterectomy, or both procedures (33).
Another risk of myomectomy is the possibility of undergoing an unexpected hysterectomy because of intraoperative complications. This risk appears to be low (less than 1%) even when uterine size is substantial (28, 34-37). Blood loss and the risk of transfusion may be increased in women with larger uteri (28, 37).
Pooled data from several case series of laparoscopic myomectomy involving more than 750 pregnancies identified one case of uterine rupture (39, 40, 75-77). Other case reports have described the occurrence of uterine rupture before and during labor (78-80), including rare case reports of uterine rupture remote from term after traditional abdominal myomectomy (81, 82). Most obstetricians allow women who underwent hysteroscopic myomectomy for type O or type I leiomyomas to go through labor and give birth vaginally; however, there are case reports of uterine rupture in women who experienced uterine perforation during hysteroscopy (83-85). It appears that the risk of uterine rupture in pregnancy after laparoscopic or hysteroscopic myomectomy is low. However, because of the serious nature of this complication, a high index of suspicion must be maintained when managing pregnancies after this procedure.
